I find it odd at this juncture in late July that I’ve been writing about a certain drug that was touted as a “miracle cure” for COVID-19 as far back as March. I am referring, of course, to hydroxychloroquine, an anti-malarial drug that also has immunomodulatory effects that make it also useful to treat various autoimmune diseases, such as systemic lupus erythematosus. It’s a drug that, despite the lack of evidence for its efficacy and the continued publication of negative studies testing its efficacy against the disease, just won’t die. Truly, hydroxychloroquine is the Jason Voorhees of drugs, at least with respect to COVID-19. After each new study showing it to be ineffective, it always seems to rise, just as Jason always comes back for another round of killing after seemingly having died at the end of the previous movie.
The hypothesis that antimalarial drugs might be effective treatments for COVID-19 originated in Wuhan, China during the early phase of the pandemic in January. There, Chinese researchers reported that none of their 80 patients with lupus erythematosus who were taking hydroxychloroquine went on to become infected with SARS-CoV-2. As a result of that and old evidence of antiviral activity for the drugs, they became interested in using these antimalarial drugs to treat COVID-19. (Never mind that immunosuppressed patients are exactly the patients most likely to assiduously follow the recommendations of public health authorities during a pandemic.) A number of clinical trials were registered, and, based on anecdotal reports and small clinical trials (nearly all of which are as yet unpublished), in February the Chinese government published an expert consensus recommending CQ or HCQ for patients with COVID-19. Soon after, a number of nations followed suit. From there, a French “brave maverick scientist” named Didier Raoult latched onto the drug as the “answer” to the COVID-19 pandemic, publishing risibly bad studies claiming to show its efficacy. Tech bros such as Elon Musk discovered the claims about hydroxychloroquine and Raoult’s bad science, leading to Donald Trump Tweeting favorably about his study and, ultimately, to the FDA issuing an emergency use authorization for the drug to treat COVID-19.
Since then, there has been a drip-drip-drip of negative studies of hydroxychloroquine, some studies observational, but, increasingly, many being randomized clinical trials, such as the publication of a randomized controlled clinical trial of the drug as post-exposure prophylaxis that was entirely negative. This was followed by two more, first, a Spanish post-exposure prophylaxis trial that was also negative. Then there was the Recovery Trial from the UK, which failed to find a benefit from hydroxychloroquine in hospitalized patients treated with the drug, leading to the revocation of the FDA’s original ill-advised EUA.
Despite the weight of the negative evidence that’s been accumulating, for some reason, last week the advocates of hydroxychloroquine as a treatment for COVID-19 have been doubling down. You might think that they’d slink off and pretend that the negative evidence hasn’t been accumulating. To quote John Belushi, “But nooooo!” No, they have to double down. I’m going to look at two examples. The first one is particularly disappointing, as it involves an apparently respected epidemiologist. The second is less so, given that it involves the crank medical “society” known as the Association of American Physicians and Surgeons (AAPS), a group featured on this very blog more than once before.
Harvey Risch: Defending hydroxychloroquine with bad science
I’m generally a big fan of epidemiology and epidemiologists. After all, epidemiology is how we know that tobacco smoking causes cancer and that vaccines do not cause autism, sudden infant death syndrome, autoimmune diseases, diabetes, or the other conditions and diseases attributed to vaccines by antivaxxers. Epidemiology is also how we will ultimately figure out who is at most risk for serious disease, complications, and death from COVID-19 and then use that information to fine-tune the public health response to the pandemic and to develop additional interventions. So I scratched my head mightily yesterday when I saw an op-ed in Newsweek by Harvey Risch, MD, PhD, a professor of epidemiology at the Yale School of Public Health entitled “The Key to Defeating COVID-19 Already Exists. We Need to Start Using It“. What is this “key” that Risch is talking about? Hydroxychloroquine. No, seriously, I kid you not. He’s talking about what I’ve started calling the “acupuncture of the COVID-19 pandemic”:
As professor of epidemiology at Yale School of Public Health, I have authored over 300 peer-reviewed publications and currently hold senior positions on the editorial boards of several leading journals. I am usually accustomed to advocating for positions within the mainstream of medicine, so have been flummoxed to find that, in the midst of a crisis, I am fighting for a treatment that the data fully support but which, for reasons having nothing to do with a correct understanding of the science, has been pushed to the sidelines. As a result, tens of thousands of patients with COVID-19 are dying unnecessarily. Fortunately, the situation can be reversed easily and quickly.
I am referring, of course, to the medication hydroxychloroquine. When this inexpensive oral medication is given very early in the course of illness, before the virus has had time to multiply beyond control, it has shown to be highly effective, especially when given in combination with the antibiotics azithromycin or doxycycline and the nutritional supplement zinc.
This far into the pandemic, with double-blind, randomized, controlled clinical trials starting to be published and showing, each and every one of them so far, that hydroxychloroquine shows no benefit versus COVID-19 (I’ll discuss them shortly), let’s just say that I am flummoxed to find, in the midst of a crisis, that a seemingly respected epidemiologist is fighting for a drug that almost certainly doesn’t work based on low quality and anecdotal evidence when far higher quality evidence is becoming available and even the bulk of the observational evidence has been negative, with one notable outlier. I am even more flummoxed to find that Newsweek provided this epidemiologist a platform to promote this argument, particularly given how he based it primarily on a commentary and review that he wrote in May, which is basically ancient history as far as the evidence base for hydroxychloroquine goes.
Next up, Risch uses an appeal to authority—his, and that of an epidemiology journal:
On May 27, I published an article in the American Journal of Epidemiology (AJE) entitled, “Early Outpatient Treatment of Symptomatic, High-Risk COVID-19 Patients that Should be Ramped-Up Immediately as Key to the Pandemic Crisis.” That article, published in the world’s leading epidemiology journal, analyzed five studies, demonstrating clear-cut and significant benefits to treated patients, plus other very large studies that showed the medication safety.
This sort of appeal to the respectability of a scientific journal just makes me laugh these days. Journals far more prestigious than AJE have published utter rubbish before, for example The Lancet‘s publication of Andrew Wakefield‘s case series and that awful Surgisphere study on hydroxychloroquine in May. I could go on and name many other bad or even fraudulent papers in many other journals, but instead I’ll just refer to Retraction Watch for a sampling. The point is simple. Being published in a respected journal is not a guarantee of quality or that the study is even right. Indeed, I often point out that the highest profile journals, the ones that publish the most bleeding edge research, probably have a higher rate of studies that turn out to be wrong, because that’s what happens on the bleeding edge of science. Surely the eminent Prof. Risch knows this, but he makes the appeal anyway.
Since Prof. Risch referenced his own opinion article in AJE, I figured that I had to go and take a look at it. At this point, Newsweek annoyed the crap out of me because there was no direct link to the article, forcing me to go to the extra step of Googling its title and finding the article. Come on, Newsweek! It’s 2020! There’s no excuse for not including a direct link to the source and hasn’t been for at least a decade! Here, by the way, is the direct link. At this point, I would also like to point out that Prof. Risch is on the editorial board of AJE, a fact conveniently not mentioned in his Newsweek op-ed that is highly relevant, given that editorial board members can exercise a lot of influence on what gets published in a journal.
Reading the article, I was struck at how weak the arguments were. Prof. Risch basically tries to compare hydroxychloroquine to remdesivir, which I discussed nearly three months ago, when the results of the first randomized clinical trial (RCT) was announced, in essence, by press release. And, guess what? I’m not that impressed with the evidence for remdesivir’s efficacy against COVID-19, either!
Funny, though, until recently, hydroxychloroquine cultists were claiming that the drug would be effective against COVID-19 in seriously-ill hospitalized patients and then, as evidence accumulated that it isn’t, pivoted to the argument that it has to be given as early as possible in order to work. Clearly, there is a double standard at work here that Prof. Risch is not acknowledging. (We wouldn’t want to suggest that goalposts are being moved, would we?) Moreover, his argument is bullshit, plain and simple. If a drug strongly inhibits coronavirus replication, there’s no reason that it couldn’t be effective both in advanced disease and in early disease—or even as a prophylactic treatment to prevent infection. It’s true that it might not work as well (or at all) in all those situations, and it’s even true that one treatment is unlikely to work as well (or at all) in all those clinical situations, but there’s no a priori scientific reason to make the blanket declaration that one treatment can’t possibly be useful in both situations.
Think of it this way. The life-threatening inpatient acute respiratory distress syndrome caused by SARS-CoV-2 is on a continuum of disease, not a completely different disease, from symptomatic outpatient infection. In any event, I also agree that, because remdesivir hasn’t been studied in outpatient use, its use in outpatients is currently not that well supported, but, then, it is an intravenous medication only at present, making this argument rather a straw man and a red herring.
The rest of Prof. Risch’s AJE article is a veritable Gish gallop of cherry-picked studies. Hilariously, he relies heavily on uncontrolled “studies” and case series from two grifters, Didier Raoult and Vladimir Zelenko. I’ve written about Didier Raoult, a “brave maverick” true believer in his combination of hydroxychloroquine and azithromycin and a bully, on several occasions, starting with his truly execrable study claiming that his combination of hydroxychloroquine and azithromycin cleared coronavirus in all patients. None of these studies were controlled or randomized. Unbelievably, Prof. Risch cites Raoult’s case series of 1,061 COVID-19 patients as though it were anything but singularly uninformative and useless for evaluating whether his drug combination is effective against COVID-19. The results published as a preprint aren’t any more useful or convincing, either.
That’s not the most embarrassing thing in Prof. Risch’s article, though. This is:
The first study of HCQ+AZ (24) was controlled but not randomized or blinded, and involved 42 patients in Marseilles, France. This study showed a 50-fold benefit of HCQ+AZ vs standard-of-care, with P-value=.0007. In the study, six patients progressed, stopped medication use and left the trial before the day-6 planned outcome measure of swab-sampled nasopharyngeal viral clearance. Reanalysis of the raw study data elsewhere (25) and by myself shows that including these six patients does not much change the 50-fold benefit. What does change the magnitude of benefit is presentation with asymptomatic or upper respiratory-tract infection, vs lower respiratory-tract infection, the latter cutting the efficacy in half, 25-fold vs standard-of-care. This shows that the sooner these medications are used, the better their effectiveness, as would be expected for viral early respiratory disease. The average start date of medication use in this study was day-4 of symptoms. This study has been criticized on various grounds that are not germane to the science, but the most salient criticism is the lack of randomization into the control and treatment groups. This is a valid general scientific criticism, but does not represent epidemiologic experience in this instance. If the study had shown a 2-fold or perhaps 3-fold benefit, that magnitude of result could be postulated to have occurred because of subject-group differences from lack of randomization. However, the 25-fold or 50-fold benefit found in this study is not amenable to lack of randomization as the sole reason for such a huge magnitude of benefit. Further, the study showed a significant, 7-fold benefit of taking HCQ+AZ over HCQ alone, P-value=.035, which cannot be explained by differential characteristics of the controls, since it compares one treatment group to the other, and the treated subjects who received AZ had more progressed pneumonia than the treated subjects receiving HCQ alone, which should otherwise have led to worse outcomes. The study has also been described as “small,” but that criticism only applies to studies not finding statistical significance. Once a result has exceeded plausible chance finding, greater statistical significance does not contribute to evidence for causation (26).
I had a hard time believing that an actual professor of epidemiology at a school as reputable as Yale could write such drivel. The study he is referring to is Gautret et al., a study so awful, so full of flaws (and maybe even fraudulent), that it was quite properly dragged on science and medical Twitter for days and weeks afterward. That Prof. Risch would cite such an abomination of science tells you all you need to know about him.
Next, Prof. Risch cites Vladimir Zelenko. No, seriously, an epidemiologist is citing an unethical case series that hadn’t even been published yet in May. The link he provides in the citation is a link to a Google Documents page that no longer exists and was last accessed in April. I suspect that this was probably the same spreadsheet of patients that Zelenko had posted in early April that looked like this. I’m now leaning towards Prof. Risch’s commentary having not been peer-reviewed, because if an AJE peer reviewer let an author cite a link to a Google Document and call it a “two-page report,” its peer review sucks, and its editor should be ashamed of himself for publishing this. Zelenko’s evidence is so crappy that anyone citing it seriously should be thoroughly mocked.
The fourth study cited by Prof. Risch is the Prevent Senior study carried out in Brazil. It, too, was an awful study, as outlined by Elisabeth Bik. There was no randomization and no good documentation if the patients actually had COVID-19 or not. The two groups compared were not equally sick, and the reasons for hospitalizations and deaths were not listed. Moreover, the study was performed by an insurance company in Brazil which was promoting its telemedicine app for COVID-19:
2/ The study is performed from an insurance company in Brazil which has promoted its telemedicine application for #COVID19 ! So they have an interest to show efficacy of telemedicine against COVID19. the fact they have declared no COI is a joke https://t.co/Hz2DTjgeim pic.twitter.com/z1Md7ZJShK
— Dr Gaetan Burgio @[email protected] (@GaetanBurgio) April 18, 2020
But back to the Newsweek op-ed:
Since publication of my May 27 article, seven more studies have demonstrated similar benefit. In a lengthy follow-up letter, also published by AJE, I discuss these seven studies and renew my call for the immediate early use of hydroxychloroquine in high-risk patients. These seven studies include: an additional 400 high-risk patients treated by Dr. Vladimir Zelenko, with zero deaths; four studies totaling almost 500 high-risk patients treated in nursing homes and clinics across the U.S., with no deaths; a controlled trial of more than 700 high-risk patients in Brazil, with significantly reduced risk of hospitalization and two deaths among 334 patients treated with hydroxychloroquine; and another study of 398 matched patients in France, also with significantly reduced hospitalization risk. Since my letter was published, even more doctors have reported to me their completely successful use.
This is painful to read. Seriously, this is an epidemiologist? Apparently so, but he’s an epidemiologist who confuses correlation with causation:
Beyond these studies of individual patients, we have seen what happens in large populations when these drugs are used. These have been “natural experiments.” In the northern Brazil state of Pará, COVID-19 deaths were increasing exponentially. On April 6, the public hospital network purchased 75,000 doses of azithromycin and 90,000 doses of hydroxychloroquine. Over the next few weeks, authorities began distributing these medications to infected individuals. Even though new cases continued to occur, on May 22 the death rate started to plummet and is now about one-eighth what it was at the peak.
A reverse natural experiment happened in Switzerland. On May 27, the Swiss national government banned outpatient use of hydroxychloroquine for COVID-19. Around June 10, COVID-19 deaths increased four-fold and remained elevated. On June 11, the Swiss government revoked the ban, and on June 23 the death rate reverted to what it had been beforehand. People who die from COVID-19 live about three to five weeks from the start of symptoms, which makes the evidence of a causal relation in these experiments strong. Both episodes suggest that a combination of hydroxychloroquine and its companion medications reduces mortality and should be immediately adopted as the new standard of care in high-risk patients.
An Epidemiology 101 student should be able to dismantle the argument above. This is the sort of argument antivaxxers make, such as that the expansion of the vaccine schedule in the early 1990s was followed by a rise in the prevalence of autism, or claims that nations with more vaccines in their recommended schedule have higher infant mortality rates. The question to ask is: What else happened around the times that the magic drug hydroxychloroquine was disbursed to Pará or taken away from Switzerland? But, no. Whatever changes in COVID-19 mortality we’re observed must be due to the magic drug. Also, which is it? I thought that the addition of azithromycin, zinc, or doxycycline to the hydroxychloroquine was important!
It amuses me that on the very same day that Prof. Risch published his Newsweek op-ed, the New England Journal of Medicine published a clinical trial of 667 patients with mild-to-moderate COVID-19 randomized to receive placebo or hydroxychloroquine (with and without azithromycin, yet!), with the primary outcome being clinical status at 15 days. Can you guess what the result was? (Sure, I knew you could.) It was completely negative. But, wait! I can see Prof. Risch countering with the observation that this was a trial of hospitalized patients. We have that covered too! One week ago yet another randomized controlled trial of hydroxychloroquine was published in Clinical Infectious Diseases. It was a Spanish trial of 293 non-hospitalized patients with mild COVID-19, exactly the sort of study that Prof. Risch wanted. Guess what? It was negative. No benefit was observed with HCQ beyond the usual care. It is true that both of these studies did have one significant weakness, namely that they were both open label, but open-label randomized trials are still way better in terms of determining the efficacy of a drug than any of the crappy observational studies cited by Prof. Risch to argue that everyone should be getting hydroxychloroquine now. One could even argue that the trials were underpowered to detect smaller effects, but Prof. Risch is not claiming small effects on mortality. He’s claiming that hydroxychloroquine is a game changer that could save hundreds of thousands of lives!
The AAPS enters the fray
Regular readers are probably familiar with an organization known as the Association of American Physicians and Surgeons (AAPS) and its journal, the Journal of American Physicians and Surgeons (JPANDS). Basically, AAPS is a far right-wing/libertarian advocacy organization disguised as a medical professional society. When I first discovered this group, I noted that it was pretty much a fusion of a John Birch Society-like right wing group with a medical society and that it trafficked in the most vile antivaccine misinformation (e.g., that shaken baby syndrome is a “misdiagnosis” for vaccine injury and Andrew Wakefield’s recent claim that the measles vaccine will result in a mass extinction of humans), anti-immigrant fear-mongering, climate science denial, blaming breast cancer on abortion using execrable “science,” and more, such as the claim that radiation from the Fukushima reactor breach is good for you. The AAPS views doctors as some sort of mythical brave mavericks outside the herd whose godlike total autonomy must never be infringed by the government or anything else and rejects even the concept of a scientific consensus about anything. (Donald Trump’s first Secretary of Health and Human Services, Tom Price, is a member of AAPS.) Earlier this year, it even sued to protect its “right” to promote antivaccine misinformation.
Unsurprisingly, AAPS is all on board with hydroxychloroquine as a “miracle cure” for COVID-19, to the point that it’s even filed a lawsuit against the FDA! (Here are the original and follow-up filings.) Now here’s the hilarious part:
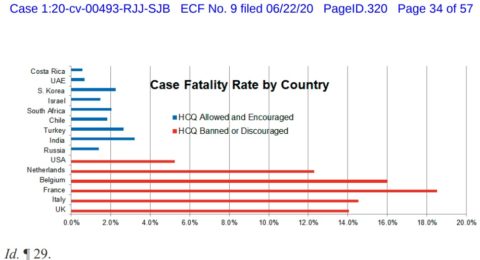
AAPS files with the court a chart showing how countries that encourage HCQ use, such as South Korea, India, Turkey, Russia, and Israel, have been far more successful in combatting COVID-19 than countries that have banned or discouraged early HCQ use, as the FDA has. Last week the FDA even misled the public by falsely stating that HCQ should not be used to treat COVID-19, when multiple studies show its benefits, and thousands of patients have been successfully treated worldwide.
“The interference with public access to hydroxychloroquine is disrupting our political processes,” notes AAPS General Counsel Andrew Schlafly. “Perhaps that is what some want, in order to deter Americans from attending political conventions and even voting, but it is unconstitutional for the FDA to infringe on these constitutional rights by blocking access to this safe medication.”
No, seriously, that’s the chart. I have so many questions and observations, too:
- This is a relatively small group of countries. There is no evidence that they were randomly selected. On what basis were they selected for this chart? I sense cherry picking.
- Given that hydroxychloroquine was (and still is) unproven, any mass adoption of the drug likely followed increases in fatalities and cases, and almost certainly was a step that was taken after other steps such as lockdowns, greatly increased testing, social distancing, etc. Isn’t it likely that the hydroxychloroquine adoption increased after these countries’ deaths/cases peaked and after they had taken other known steps that reduced measures of mortality rates (such as increased and broader testing)?
- More importantly, there are probably dozens of other factors that correlate with “country starts administering hydroxychloroquine to COVID-19 patients in large numbers”. In other words, what are the confounders?
This whole “analysis” (if you can call it that) reminds me very much of the time when antivaxxers published a truly awful study that “correlated” the number of recommended vaccines in a country’s vaccine schedule with the country’s infant mortality rate.
One also can’t help but note that AAPS has also falsely claimed that masks and social distancing are not effective in slowing the spread of COVID-19. So, of course, it can’t possibly be different policies with respect to lockdowns, testing, and contact tracing that explain the differences in mortality rates between countries. Of course, AAPS has to find another “reason” to explain differences between nations. Naturally, AAPS being AAPS, it cherry picked a relatively small sample of countries to make a correlation and incorrectly infer causation.
The bottom line
Hydroxychloroquine is the acupuncture of the COVID-19 pandemic. What do I mean by that? Like acupuncture, hydroxychloroquine is an intervention with a very low prior plausibility (although, in fairness, the prior plausibility of acupuncture is much lower than even that of hydroxychloroquine) whose cultists behave just like acupuncture cultists when it comes to evidence. They believe their magic treatment works; so, like acupuncturists, they tend to downplay accumulating evidence from double-blind, placebo-controlled trials and point to much poorer quality observational studies, while making excuses like these, described for a similar situation, the use of vitamin C to treat cancer:
Because I’m dedicated to evidence and science when it comes to medical decision making, I always concede that it is still possible that hydroxychloroquine might still be found to have some anti-COVID-19 activity, although it’s becoming increasingly clear that, if there is any activity it will likely be very modest and require large clinical trials to detect, to the point where it’ll probably be clinically insignificant. That being said, it’s amazing how much believers in acupuncture, vitamin C to treat cancer, and hydroxychloroquine to treat COVID-19 have in common. It’s also distressing how much like the villain in a slasher flick the drug is. No matter how many times it appears to have died, it always comes back.